The human body is an intricate network of systems, with each influencing the other. One of the most intriguing intersections emerging from contemporary research is the connection between our gut microbiota and mental health. This relationship, often referred to as the gut-brain axis, suggests novel potential treatments and interventions for various mental health disorders.
The Gut Microbiome Defined
Our gut is home to trillions of microorganisms, including bacteria, viruses, and fungi. This community is termed the gut microbiome. Everyone possesses a unique microbial fingerprint shaped by genetics, diet, and environmental factors from birth. [1]
Gut-Brain Axis: A Two-Way Communication
Historically, the gut and brain were viewed as distinct systems. However, modern research paints a picture of a bi-directional communication system. The gut conveys messages to the brain via neural, endocrine, immune, and metabolic pathways, and conversely, the brain communicates with the gut. [2]
Gut Microbiota’s Influence on Mental Health
Emerging studies highlight that the composition of the gut microbiome can significantly influence our mental well-being:
1. Depression and Anxiety: Research has indicated differences in gut microbiota composition between individuals with depression or anxiety and those without. [3] Some gut bacteria produce neurotransmitters like serotonin and dopamine that are essential for mood regulation.
2. Stress: Chronic stress can alter the microbiome, leading to diminished microbial diversity. This shift can affect mental health. Additionally, certain gut bacteria can produce stress hormones, intensifying this response. [4]
3. Neurodevelopmental Disorders: Preliminary research indicates a potential link between the gut microbiome and conditions such as autism spectrum disorder. [5]
The Role of Diet, Probiotics and Supplements
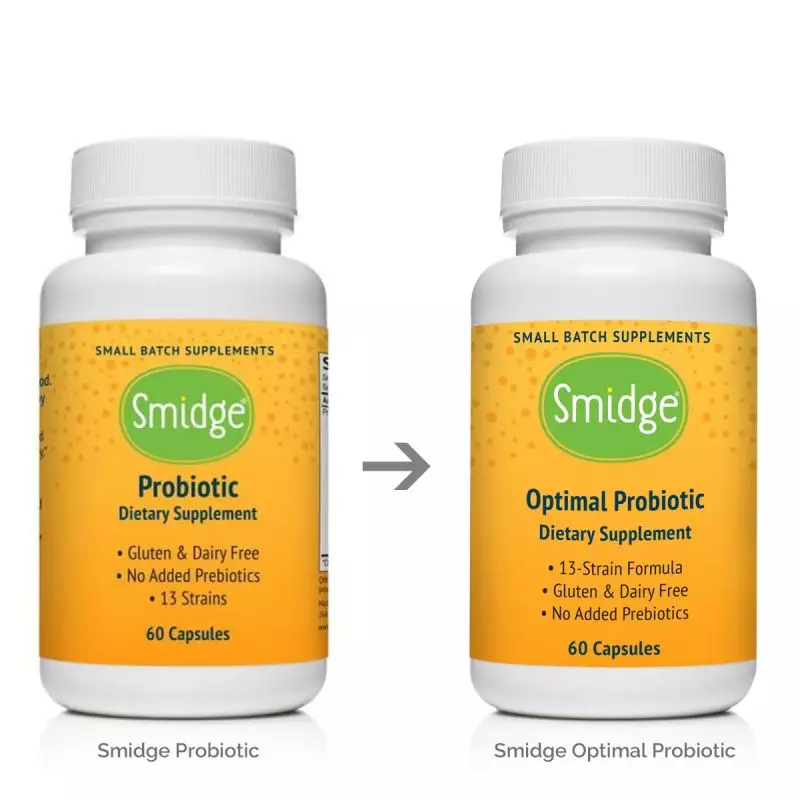
The intricate connection between the gut and the brain underscores the importance of dietary choices and gut-focused supplements in shaping mental health. As research expands, targeted supplements, especially probiotics and digestive enzymes, are becoming central players in this arena.
These products highlight this emerging focus:
• Smidge Sensitive Probiotic Powder: This finely-tuned probiotic powder is tailored especially for those with sensitive digestive systems. By offering a blend of beneficial bacterial strains, Smidge works diligently to nurture a balanced gut environment. A healthy gut microbiome is intricately connected to mood regulation and overall mental health.
• Smidge Digestive Enzymes: Enzymes play a crucial role in breaking down food and ensuring optimal nutrient absorption. Smidge Digestive Enzymes are designed to support this process, promoting gut health and, by extension, contributing to mental well-being.
Consistent intake of such supplements, coupled with a balanced diet, can aid in optimising the gut environment, possibly leading to improved mental health outcomes. [6]
As always, before introducing new supplements, it's vital to consult with a healthcare professional to ensure they align with your individual health needs.
Challenges and Future Directions
There remain several challenges:
1. Causation vs Correlation: It's still being debated whether changes in microbiota composition cause mental health issues or vice versa.
2. Standardisation of Probiotics: The effects of probiotics can be strain-specific, making generalisations difficult. [7]
3. Diet Complexity: Diet encompasses multiple facets, making it challenging to identify specific components that affect mental health.
Yet, the rapid pace of research offers hope for clearer insights and interventions in the near future.
Conclusion
The exploration of the gut microbiome and its influence on mental health reveals our body’s complex interconnectedness. Though research is still ongoing, our gut health undeniably plays a critical role in mental well-being.
References:
1 Revised Estimates for the Number of Human and Bacteria Cells in the Body
2 The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems
3 Altered fecal microbiota composition in patients with major depressive disorder
4 Exposure to a social stressor disrupts the community structure of the colonic mucosa-associated microbiota
5 Reduced Incidence of Prevotella and Other Fermenters in Intestinal Microflora of Autistic Children
6 The effects of probiotics on depressive symptoms in humans: a systematic review
7 Nutrition and mental health: A review of current knowledge about the impact of diet on mental health
Note: The article is intended for informational purposes. For medical advice or information about specific products, it's advised to consult with healthcare professionals or refer directly to the product manufacturers.

 AU Store
AU Store  UK Store
UK Store NZ Store
NZ Store EU Store
EU Store